Guía de alimentos para el embarazo

Nutrition during pregnancy isn’t exactly the same as a “normal” diet. For example, during at least the last six months of pregnancy, women should consume at the minimum 300 additional nutrient-rich calories per day, according to the U.S. Library of Medicine. Ever wonder why eating sushi is considered taboo during pregnancy? Certain foods that are normally considered healthy may be harmful to your growing baby. Here’s why.
Many soft cheeses such as queso blanco, Brie, Camembert and feta are made with unpasteurized milk, and can contain the Listeria monocytogenes bacterium, which causes an infection known as listeriosis that may lead to miscarriage, premature birth or stillbirth. According to the Centers for Disease Control and Prevention (CDC), cheeses are up to 160 times more likely to cause listeriosis when made with unpasteurized milk. Some soft cheese labels say they’re made with pasteurized milk, but even these cheeses have caused infections, so it’s better to steer clear.
Some types of fish contain high levels of methylmercury, a neurotoxin that can hurt an unborn baby’s developing nervous system and has been linked with developmental problems. The Food and Drug Administration recommends pregnant women avoid shark, swordfish, king mackerel and tilefish. You should also limit sushi, as raw fish is more likely to cause foodborne illnesses. More Information below.
Deli meats can also become contaminated with Listeria, even though the meat is cooked. That’s because contamination can occur after the meat is cooked but before it’s packaged. According to the CDC, 1,700 cases of Listeria infection occur every year in the United States, and pregnant women and newborns are especially vulnerable.
Alcohol from wine, beer or liquor can easily pass through the placenta to the baby. Exposure to alcohol increases the baby’s risk of developing a birth defect or a fetal alcohol spectrum disorder (FASD). FASDs include a range of behavioral and developmental problems, including fetal alcohol syndrome. Drinking even small amounts of alcohol while pregnant can lead to fetal harm or death, according to the American Academy of Pediatrics.
The safe level of alcohol consumption is unknown. Consuming alcohol during pregnancy increases the risk of miscarriage, low birth weight, congenital deformities and effects on the baby’s intelligence.
The National Health and Medical Research Council advises women that it is best not to drink during pregnancy. Australian Alcohol Guidelines recommend that women who are pregnant or who are considering pregnancy should never become ‘drunk’ and may like to consider not drinking at all. If you choose to drink, it is suggested to have less than seven standard drinks in a week and no more than two standard drinks on any one day.
There are few things as delicious as a prime cut of rare steak — the kind with a juicy, ruby-red center. Unfortunately, undercooked meat can contain harmful bacteria, such as salmonella, or a parasite called Toxoplasma gondii that causes toxoplasmosis, a serious blood infection. When toxoplasmosis passes to a fetus, it can cause premature birth, jaundice, developmental disorders and brain damage. Although infections are rare, moms-to-be should make sure their meat is cooked to a safe internal temperature. Use this list as a guide when you’re cooking meat:
- beef, pork, veal, lamb: 145° F
- ground beef, ground pork, ground veal, ground lamb: 160° F
- fish: 145° F
- ground poultry: 165° F
- poultry: 165° F
Pregnancy
Nutrition during the preconception period, as well as throughout a pregnancy, has a major impact on pregnancy outcome. Among prepregnancy considerations, the prepregnancy Body Mass Index (BMI), folic acid status, and socioeconomic status are the most important.
Prepregnancy BMI is an important factor in predicting pregnancy outcome, since both low prepregnancy and high prepregnancy BMI are associated with an increased risk for a negative pregnancy outcome.
Folic acid, a B vitamin, has been shown to prevent birth defects of the brain and spinal cord known as neural tube defects (NTDs). The most common NTDs are spina bifida and anencephaly. Folic acid is therefore needed
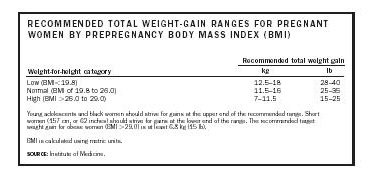
RECOMMENDED TOTAL WEIGHT-GAIN RANGES FOR PREGNANT WOMEN BY PREPREGNANCY BODY MASS INDEX (BMI)
Weight-for-height category | Recommended total weight gain | |
| kg | lb |
Young adolescents and black women should strive for gains at the upper end of the recommended range. Short women (157 cm, or 62 inches) should strive for gains at the lower end of the range. The recommended target weight gain for obese women (BMI 29.0) is at least 6.8 kg (15 lb). | ||
BMI is calculated using metric units. | ||
SOURCE: Institute of Medicine. | ||
Low (BMI 19.8) | 12.5–18 | 28–40 |
Normal (BMI of 19.8 to 26.0) | 11.5–16 | 25–35 |
High (BMI 26.0 to 29.0) | 7–11.5 | 15–25 |
both in preconception and early pregnancy. Since studies indicate that most women get less than half the recommended amount of folic acid, the March of Dimes recommends women consider a supplement of 400 micrograms of folic acid preconceptually to prevent the incidence of neural tube defects. In addition, it is suggested women capable of becoming pregnant consume a diet high in folic acid. Good sources of folic acid include oranges, green leafy vegetables, and fortified bread and cereals.
There is also a direct correlation between ethnicity, age, marital status, and educational status with increased negative pregnancy outcomes, such as low birth weight.
Pregnancy Weight Gain
Pregnancy is divided into three trimesters, with each trimester lasting three months, or approximately thirteen weeks (a normal pregnancy lasts 40 weeks). Recommendations for weight gain during pregnancy are based on the Institute of Medicine (IOM) definitions of prepregnancy BMI range. The BMI is defined as weight in pounds, divided by height in inches, divided by height in inches, multiplied by 703 (or weight in kilograms, divided by height in centimeters, divided by height in centimeters, multiplied by ten-thousand). The majority of weight gain should occur in the second and third trimesters. Weight gain can vary greatly in normal pregnancies with normal birth outcomes. Few studies have included women in their first trimester, so the importance of first-trimester weight gain on pregnancy outcome is unclear. However, a slow and steady rate of weight gain is considered ideal. The current recommended weight gain for the BMI ranges are outlined in the accompanying figure.
Poor weight gain during pregnancy is associated with prematurity, low birth weight, and small for gestational age. Among normal-weight women, weight gain above the recommended level corresponds to maternal fat stores and is not of benefit to fetal growth. In other words, fat gain during pregnancy parallels gestational weight gain, and women with greater weight gain also gain more fat. In addition, an inverse relationship exists between pre-pregnancy BMI and weight gain during pregnancy: women with a low pre-pregnancy BMI tend to gain more weight than women with a high prepregnancy BMI. On average, overweight women gain less weight than their thinner counterparts, though it is not unusual for obese women to achieve normal birth outcomes with less than the recommended weight gain.
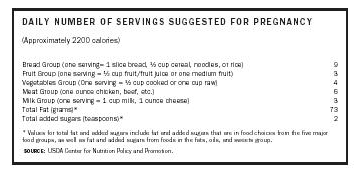
DAILY NUMBER OF SERVINGS SUGGESTED FOR PREGNANCY (Approximately 2200 calories)
* Values for total fat and added sugars include fat and added sugars that are in food choices from the five major food groups, as well as fat and added sugars from foods in the fats, oils, and sweets group. | |
SOURCE: USDA Center for Nutrition Policy and Promotion. | |
Bread Group (one serving= 1 slice bread, ½ cup cereal, noodles, or rice) | 9 |
Fruit Group (one serving = ½ cup fruit/fruit juice or one medium fruit) | 3 |
Vegetables Group (One serving = ½ cup cooked or one cup raw) | 4 |
Meat Group (one ounce chicken, beef, etc.) | 6 |
Milk Group (one serving = 1 cup milk, 1 ounce cheese) | 3 |
Total Fat (grams)* | 73 |
Total added sugars (teaspoons)* | 2 |
In adolescent pregnancies, there are no established BMI recommendations regarding prepregnancy weight and weight gain. Excess weight gain, however, has been associated with postpartum obesity in adolescents.
Pregnancy Nutrition Requirements
Traditionally, caloric requirements during pregnancy have been estimated to be around an additional 300 calories per day. However, this must be adjusted for physical activity and prepregnancy weight (see accompanying figure) for the recommended number of servings of food groups). To meet weight-gain recommendations, a woman with a low prepregnancy BMI and a high activity level would require more calories than a woman with a high prepregnancy BMI and a sedentary lifestyle . A variety of foods from all food groups is important, since foods within the same food group do not contain exactly the same amount of nutrients . If increased weight gain is recommended, an emphasis should be placed on high-calorie food group items that contain a higher fat and sugar content. When less weight gain is recommended, women should choose from the lower-calorie food group choices.
Recommendations regarding sugar intake for pregnant women depend on weight gain and maternal blood glucose levels. A high sugar intake would not be advisable for women gaining more than the recommended weight or for those women who are having difficulty controlling normal blood glucose levels, while a high sugar intake would be beneficial for women requiring increased weight gain. A high sugar intake for women who are experiencing excessive weight gain or having difficulty maintaining normal glucose levels could result in increased maternal risk for complications associated with too much weight gain, such as diabetes , hypertension , premature delivery, and a large for gestational age fetus.
Adequate fluid intake is important to maintain hemodynamics (blood circulation) and homeostasis (fluid and tissue balance) and to reduce the risk of urinary tract infections. All pregnant women are encouraged to consume at least 64 ounces of fluid daily. Women at risk of gaining too much weight should be cautioned to limit their intake of sweetened fluids, including juice, and to consume more water. Exercise is considered healthful for most pregnant women, who should be encouraged to continue to exercise at prepregnancy levels. However, women should be cautious about
![This human fetus is in the second trimester of development, a time when fetal weight gain begins to accelerate. Pregnant women should increase caloric intake by approximately 300 calories per day to account for rapid fetal growth. Calcium and iron supplements may also be necessary. [Photo Researchers, Inc. Reproduced by permission.]](https://cdn-cms.f-static.net/uploads/3382921/2000_5f5010f3ac5bd.png)
This human fetus is in the second trimester of development, a time when fetal weight gain begins to accelerate. Pregnant women should increase caloric intake by approximately 300 calories per day to account for rapid fetal growth. Calcium and iron supplements may also be necessary.
[Photo Researchers, Inc. Reproduced by permission.]
beginning any new exercise program during pregnancy, and, if medically advised, should avoid certain activities. Health care providers may recommend bed rest and limiting physical activity (such as work) when preterm labor is present or when weight gain is poor. Increased physical activity will control excess weight gain, in addition to the normal beneficial physical and emotional effects.
Vitamin and Mineral Requirements
Iron is the only recommended nutrient for which requirements cannot be reasonably met by diet alone during pregnancy. Thirty milligrams of ferrous iron is recommended, and iron should be taken on an empty stomach. When more than 30 mg of iron is given to treat anemia , it is suggested to also take approximately 15 mg of zinc and 2 mg of copper, since iron interferes with absorption and utilization of these materials.
According to some studies, caffeine decreases the availability of certain nutrients, such as calcium , zinc, and iron. Current recommendations, therefore, include limiting the consumption of caffeinated containing products.
Calcium supplementation may be suggested if the average daily intake of calcium is less than 600 mg. Calcium intake is of particular concern among pregnant women under the age of twenty-five, since bone mineral density is still increasing in these women. Calcium supplements, if recommended, should be taken with meals. Additionally, vitamin D may be necessary if sunlight exposure is minimal. For vegetarians, the current recommendations also include a daily supplement of 2 mg of Vitamin B 12 .
For women who don't ordinarily consume an adequate diet, or for those in high-risk categories (such as those carrying twins, heavy smokers, and drug abusers) a prenatal vitamin supplement is recommended, beginning in the second trimester. The supplement should contain the following: iron (30 mg); zinc (15 mg); copper (2 mg); calcium (250 mg); vitamin B 6 (62 mg); folate (300 mg); vitamin C (50 mg); vitamin D (5 mg).
Special Nutrition Concerns
Food cravings during pregnancy are common and are not cause for concern, provided other nutrient needs are met and weight gain is in the target range. Pica—the ingestion of nonfood substances of nutritional value—is associated with anemia and can be a source of lead poisoning, bacterial infection, and dental problems. Pregnant women should be encouraged to avoid pica and discuss it with their medical provider.
Gestational diabetes is associated with high prepregnancy BMI and excess pregnancy weight gain. Infants of gestational-diabetic mothers are usually born large for gestational age (macrosomia) and are at higher risk for cesarean delivery and hypoglycemia postpartum.
Symptoms of toxemia of pregnancy, also known as preeclampsia, include swelling ( edema ) and proteinuria (excess protein in the urine). The cause of toxemia has not been determined, but the risk is associated with first pregnancies, advanced maternal age, African-American ethnicity, and women with a past history of diabetes, hypertension, or kidney disease. In severe cases, delivery is frequently induced.
Tips for common pregnancy discomforts include avoidance of offending foods (and their odor) when nausea and heartburn occur. Many pregnant women find that spicy, fatty foods can increase problems with nausea and heartburn. Frequent, small, and blander meals are often better tolerated. Some women find eating dry crackers before rising from bed in the morning helpful for nausea. However, since nausea and vomiting usually subside by the end of the first trimester, they do not have a significant impact on the final weight gain in most pregnancies. Hyperemesis gravidarum, or intractable vomiting during pregnancy, can rapidly result in dehydration , so medical intervention is required.
When constipation is a concern, increased consumption of whole grains, fruits, and vegetables is advisable, as well as increased fluid intake and physical activity.
Breastfeeding is the recommended method of infant nutrition, with a few exceptions. It benefits both mother and infant by providing protective antibodies to human disease, and breastfed babies are generally healthier and have higher I.Q. levels than bottle-fed babies. The development of jaw alignment problems and allergies are also far less likely in breastfed babies, while mothers who breastfeed have less postpartum complications and are considered to be at lower risk for breast cancer .
In the United States, women with HIV infection should not breastfeed. This is not a contraindication in developing countries, however, as the benefits may outweigh the possibility of infection. Untreated tuberculosis is also a contraindication for breastfeeding, while hepatitis C is currently not a contraindication for breastfeeding.
The Women, Infants, and Children (WIC) Program
The WIC program was established in the 1970s as a supplemental food and nutrition-education program. Eligibility requirements include a household income of up to 185 percent of the federal poverty level, as well as nutrition-risk criteria. The WIC program goals include improving pregnancy outcomes by helping participants achieve recommended weight gain. Nutritional food choices and calorie levels based on recommended weight gain are emphasized. The program has been shown to significantly reduce a number of negative pregnancy outcomes, including low birth weight.
Pregnancy creates extra demands on the body for nutrients such as protein, iron, folate and iodine. Pregnant women need to focus on boosting their nutritional intake, rather than their energy (kilojoule) intake. A folic acid (folate) supplement should be taken prior to conception and for the first three months of pregnancy to reduce the risk of neural tube defects such as spina bifida. Small regular snacks may help nausea or morning sickness.
Good nutrition during pregnancy will help to keep a developing baby and its mother healthy. The need for certain nutrients, such as iron and folate, is increased at this time but only a small amount of extra energy (kilojoules) is needed.
If you are pregnant, a good approach is to eat to satisfy your appetite and continue to monitor your weight. A normal weight gain over the course of a pregnancy is around 10–13kg for women who have a healthy pre-conception weight.
A varied diet generally provides our bodies with enough of each vitamin and mineral each day. However, pregnant women may need supplements of particular vitamins or minerals. Be advised by your doctor before taking supplements.
Healthy foods for pregnant women
It is important to choose a wide variety of foods to ensure the nutritional needs of both mother and baby are met. Try to eat:
Lots of fruit and vegetables, wholegrain breads and cereals
Moderate amounts of low fat dairy foods and lean meats
Small amounts of foods high in fat, sugar and salt
Lean meat, chicken and fish
Dried beans and lentils
Nuts and seeds
Green leafy vegetables.
Folic acid (folate)
Folate (known as folic acid when added to foods) is a B-group vitamin found in a variety of foods. Some breakfast cereals, breads and juices are fortified with folic acid. This will be listed on the nutrition label of these products.
As well as a healthy diet, it is recommended that women planning a pregnancy take a folic acid supplement prior to conception and for the first three months of pregnancy to reduce the risk of neural tube defects such as spina bifida. Folate taken over this period can prevent up to seven out of 10 cases of neural tube defects.
If you are planning a pregnancy or are in the early stages of pregnancy, you should increase your folate intake by an additional 0.4mg (400µg) per day above the recommended daily intake (RDI) of 0.6mg (600µg) per day for pregnancy.
Folate in your diet
Excellent food sources of folate include:
Asparagus
Bran flakes
Broccoli
Brussels sprouts
Chick peas
Dried beans
Lentils
Spinach.
Very good food sources of folate include:
Cabbage
Cauliflower
Leeks
Oranges
Orange juice
Parsley
Peas
Wheat germ
Wholegrain bread.
Good food sources of folate include:
Hazelnuts
Vegemite
Parsnips
Potato
Salmon
Strawberries
Tomato
Unsalted peanuts
Walnuts.
Although liver is high in folate, it is not recommended to women who are, or could be pregnant, because of its high vitamin A content.
Iron
Pregnancy increases the need for iron in the diet. The developing foetus draws enough iron from the mother to last it through the first five or six months after birth so a woman has an increased need for iron during pregnancy.
Iron losses are reduced during pregnancy because the woman is no longer menstruating and so loses less iron from menstrual blood loss. It is useful to include foods that are good sources of iron in the diet every day (for example red meat) and to have foods that are good sources of vitamin C (like oranges) to help absorb the iron.
The recommended daily intake (RDI) of iron during pregnancy is 27mg per day (9mg per day more than that for non-pregnant women). The amount needed depends on the amount of iron the woman has ‘stored’ in her body prior to pregnancy. If your iron stores are very low, you may need to get more from supplements. It is important to discuss your need for supplements with your doctor, as iron can be toxic in large amounts.
Iodine
Iodine is an important mineral needed for the production of thyroid hormone, which is important for growth and development. Inadequate iodine intake during pregnancy increases the risk of mental impairment and cretinism in the newborn baby.
Foods that are good sources of iodine include seafood and seaweed (including nori and kelp), eggs, meat and dairy products. Women who are pregnant should also use iodised table salt when cooking or adding salt to food.
Vitamin A
Although vitamin A requirements do increase during pregnancy, vitamin A supplements are rarely recommended for pregnant women. This is because an excessive intake of vitamin A may cause birth deformities.
The best way to increase your intake of vitamin A, if it is low, is through food sources like milk, fish, eggs and margarine.
Multivitamin supplements
Multivitamin supplements may be recommended for the following groups of pregnant women:
Vegetarians
Teenagers who may have an inadequate food intake
Substance misusers (of drugs, tobacco and alcohol)
Obese pregnant women who are restricting their energy intake to prevent large weight gains.
Always be advised by your doctor before taking vitamin or mineral supplements.
There is no need for extra calcium during pregnancy
Until 2006, Australian dietary recommendations advised increased calcium intake during pregnancy and lactation. This advice has since been revised. Although there is a large ‘shift’ of calcium to the baby during the third trimester of pregnancy, as it starts to develop and strengthen its bones, the mother’s increased capacity to absorb dietary calcium makes up for this loss without the need for extra intake.
The recommended dietary intake for non-pregnant women (1,000mg per day for women aged 19–50 years and 1,300mg per day for adolescents or those aged over 51) remains unchanged during pregnancy and breastfeeding. Dairy foods, such as milk, cheese and yoghurt, and calcium-fortified soymilk are excellent dietary sources of calcium.
Eating for two
There is no need to eat more food during pregnancy. It is recommended that for the first trimester, a woman’s energy (kilojoule) intake should remain about the same as it was prior to the pregnancy. During the second and third trimesters, energy requirements should increase by about 600kJ a day. Increasing fruit intake to four serves each day (from the recommended two serves for non-pregnant women) will provide all the extra energy needed.
The dangers of dieting
Some women fear the extra weight gain of pregnancy and decide to eat sparingly to avoid putting on body fat. Restricted eating or crash dieting in any form while pregnant can seriously compromise your health and that of your baby.
Pregnancy in adolescence
Pregnant adolescents need more nutrients than adult women, because they are still growing themselves. Adolescents may give birth to smaller infants because they are competing with the growing foetus for nutrients.
Anemia is more common among adolescents than older women. Calcium intake is also important because young women have not yet reached their peak bone mass and inadequate calcium intake may increase the risk of osteoporosis developing later in life.
Nausea and vomiting
Nausea and vomiting, especially ‘morning sickness’, are common during pregnancy – particularly in the first trimester. Small carbohydrate snacks (a sandwich or fruit) every two to three hours may provide some relief. The following suggestions may also help:
Eat some dry bread, biscuits or cereal before getting up in the morning. Get up slowly, avoiding sudden movements.
Drink liquids between rather than with meals to avoid bloating as this can trigger vomiting.
Avoid large meals and greasy, highly spiced foods.
Suck something sour like a lemon.
Relax, rest and get into the fresh air as much as possible. Keep rooms well ventilated and odour free.
Slowly sip a fizzy drink when feeling nauseated.
Try food and drinks containing ginger as these sometimes relieve nausea.
Heartburn
Heartburn is common in pregnancy because, as the baby grows, there is more pressure on the abdomen. Small, frequent meals may be better than large meals. Try to avoid:
Eating late at night
Bending, lifting or lying down after meals
Excessive consumption of tea or coffee.
You may also like to try sleeping with your bedhead raised a few inches. You can do this by putting a folded blanket or pillow under your mattress.
Listeria infection
Listeria infection, or listeriosis, is an illness usually caused by eating food contaminated with bacteria known as Listeria monocytogenes. Healthy people may experience no ill-effects from listeria infection at all, but the risks are substantial for pregnant women. The greatest danger is to the unborn baby, with increased risk of miscarriage, stillbirth or premature labour. A listeria infection is easily treated with antibiotics, but prevention is best.
Some foods are more prone to contamination with listeria than others. Exclude these foods from your diet if you are pregnant:
Soft cheeses, such as brie, camembert and ricotta – these are safe if served cooked and hot
Precooked or pre-prepared cold foods that will not be reheated – for example, pre-prepared salads, paté, quiches and delicatessen meats like ham and salami
Raw seafood such as oysters and sashimi or smoked seafood such as salmon (canned varieties are safe)
Unpasteurised foods
Soft-serve icecream.
The organism that causes listeria infection is destroyed by heat, so properly cooked foods are not a risk.
Salmonella
Salmonella is a cause of food poisoning that can trigger miscarriage. The most likely sources of salmonella are raw eggs and undercooked meat and poultry.
Good food hygiene
Good food hygiene is the best way to reduce the risk of salmonella and listeria infections. Suggestions include:
Always wash your hands before and after preparing food.
Keep your kitchen surfaces clean.
Do not let uncooked food contaminate cooked food.
Wash fruit, vegetables and salad before eating.
Cook food thoroughly.
Keep pets away from kitchen surfaces.
Wear rubber gloves when handling cat litter trays or gardening.
Store food at correct temperatures.
Mercury in fish
It is suggested that pregnant women eat 2–3 serves of fish every week for the good health of themselves and their developing baby. Caution should be exercised when choosing the type of fish you will eat. There are a few types of fish that need to be limited because they contain high levels of mercury, which is dangerous for the developing fetus.
Pregnant women should:
Limit to one serve (150g) per fortnight – billfish (swordfish, broadbill and marlin) and shark (flake), with no other fish eaten in that fortnight.
Limit to one serve (150g) per week – orange roughy (deep sea perch) or catfish, with no other fish eaten that week.
Women should not be worried if they’ve had the odd meal of fish with high levels of mercury. It is only a potential problem when that type of fish is eaten regularly, which causes a build-up of mercury in the mother’s blood.
Where to get help
Your doctor
Midwife
Obstetrician
An Accredited Practising Dietitian, contact the Dietitians Association of Australia
Things to remember
A pregnant woman needs to boost her nutrient intake, rather than her kilojoule intake.
Pregnancy creates extra demands for certain nutrients including iron and folate.
Good food hygiene is particularly important during pregnancy
Helping Your Baby Start A Healthy Life
Did you know that a prenatal vitamin not only helps to prevent birth defects, but that it can also help with your child’s brain development, behavior, learning ability, and help reduce childhood obesity? You can give your baby a head start in life by simply taking a prenatal vitamin that contains a few important ingredients.
BestPrenatalVitamins.org was made to help educate people on new research that has come out on prenatal vitamins. This website can help you learn what the newest studies are saying, which ingredients to look for, and what percentage of ingredients should be found in your prenatal vitamin.
Three Must Have Ingredients
 There are three major ingredients that doctors say need to be found in every prenatal vitamin
There are three major ingredients that doctors say need to be found in every prenatal vitamin
Folate or Folic Acid- Helps to prevent neural tube defects. Neural tube defects are serious abnormalities that affect the brain and spinal cord.
Calcium- Helps strengthen bones and teeth for both mother and baby. Calcium is also important for your muscular and nervous system to run normally.
Iron- Helps support in the development in blood cells and muscle cells for both mother and baby. Iron helps to reduce anemia, a problem where the mother is lacking healthy red blood cells.
Newly Researched Ingredients
Here are a number of other ingredients that you should know about when looking into prenatal vitamins. Based on new research for infant development, these ingredients should be a must have in your prenatal vitamin.
DHA- Is an omega-3 fatty acid, which has been found in a number of studies to help promote a baby’s brain and eye development. Omega-3 fatty acids are mostly found in fish which many pregnant women choose not to eat due to the high mercury content found in fish.
Probiotics- Have been found to possibly reduce excessively large birth sizes and reduce obesity later in a child’s life. It has also shown to help the mother reduce excessive weight gain during pregnancy and helpful for reducing weight after pregnancy. On top of this probiotics have shown to reduce early childhood eczema by 46%.
Co-Q10- Studies have found that CoQ10, which is an enzyme, can reduce the risk of developing preeclampsia during pregnancy. CoQ10 also helps to promote healing after delivery.
Ginger- Helps to treat and prevent nausea and vomiting associated with morning sickness. Ginger also contains cholesterol lowering qualities.
Vitamin B6- In a study vitamin B6 has been found to reduce miscarriages and also increase the chance of conception. Vitamin B6 can also help with nausea.
Vitamin D3- Helps with bone health and density. Reduces preeclampsia. Studies have also found Vitamin D3 to help with depression.
Choline- Recent studies have found choline to increase the size of brain cells and can make brain cells faster at firing electrical signals. The study showed that choline supplementation during pregnancy could affect a baby’s lifelong learning and memory.
Inositol- In a study done at Washington School of Medicine, Inositol was found to help reduce the chance of neural tube defects. The study found that on top of Folic Acid Inositol helped to further reduce neural tube defects.
Vitamin A- Has been found to help with embryonic development and with infection resistance. Keep in mind that too much Vitamin can be a bad thing. Doses over 10,000 IU can cause fetal poisoning.
Researching a Prenatal Vitamin
When choosing a prenatal vitamin you need to know what to look for. To do this you should do some research. Don’t just trust one source of information. There are many companies that will claim a lot about their product, and produce a lot of hype about their prenatal vitamin. Even though a product may contain all the ingredients you are looking for, you may find out that they come from a poor source or that is does not contain the percentage that you and your baby need. Make sure to look into how much you need in vitamins and minerals. The list below goes over the amounts that several doctors recommend.
Recommended Daily Amounts of Ingredients
CoQ10- Look for products carrying 150-200mg of CoQ10. Few prenatal vitamins contain this ingredient.
Probiotics- Look for products containing probiotics. This is one ingredient that many prenatal vitamins do not contain. Look for a blend of at least 5 or more.
Calcium- Look for products containing at least 750mg.
Choline- Look for 20-25mg.
Folate or Folic Acid- Look for at least 400mcg, but 800-1000mcg would be best.
Vitamin B6- Most research suggests 25-50mg.
DHA- A good number is 50-200mg.
Vitamin A- Most doctors recommend getting no more than 5000 IU which is a 100% of your daily value.
Inositol- Look for 20mg-25mg.
Vitamin D3- Look for a 100% of your daily recommendation, 400 IU.
Iron- Some people may need more and some may need less, 25-30mg is what most doctors recommend.
What to Avoid In Prenatal Vitamins
Do not take prenatal vitamins that contain over 10,000 IU of Vitamin A, because of the possibility of fetal poisoning. Another thing to look for when looking into prenatal vitamins are the other ingredients found at the bottom of the ingredient list. Dyes, sweeteners, preservatives, and hydrogenated oils should be avoided.