Burch Retropubic Urethroplexi
Burch Colposuspension Treatment
Burch Colposuspension is a treatment for stress urinary incontinence (SUI) in women. The aim is to reposition the bladder neck so that it can better resist the pressure from a full bladder. Your doctor can also recommend this surgery if you suffer from mixed urinary incontinence. Because the surgery is designed to treat only SUI symptoms, it may be less effective in these cases.
When should I consider colposuspension?
Burch colposuspension is an alternative treatment to sling implantation if you have mild to moderate urinary incontinence. Because slings are the most common treatment option for SUI, colposuspension is generally only recommended if they are not the best treatment option for you.
in-depth information
How is Burch colposuspension performed?
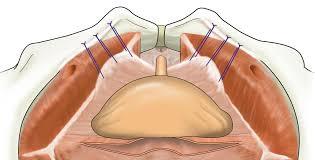
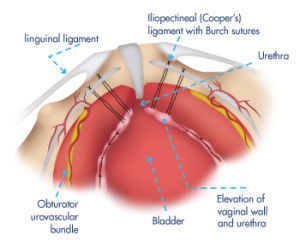
For Burch colposuspension you will receive general anaesthesia. First the surgeon inserts a catheter into your bladder, to make sure it is completely empty. Then, the top of your vaginais attached to the ligament behind your pubic bone with supporting stitches. This will lift your bladder neck (Fig. 1).
Burch colposuspension can be performed by open surgery or laparoscopic surgery. For open surgery the surgeon makes an incision in your lower abdomen to access the pelvic area directly. For laparoscopic surgery, the surgeon inserts small plastic tubes into your abdomen. Through these tubes the surgeon can insert the instruments needed to perform the surgery. One of the small tubes is used to insert a camera which allows the surgeon to see a high-quality image of the area on a video monitor (Fig. 2).
Laparoscopic and open surgery are equally effective to cure SUI in women. In general, hospital stay is shorter with laparoscopic surgery.
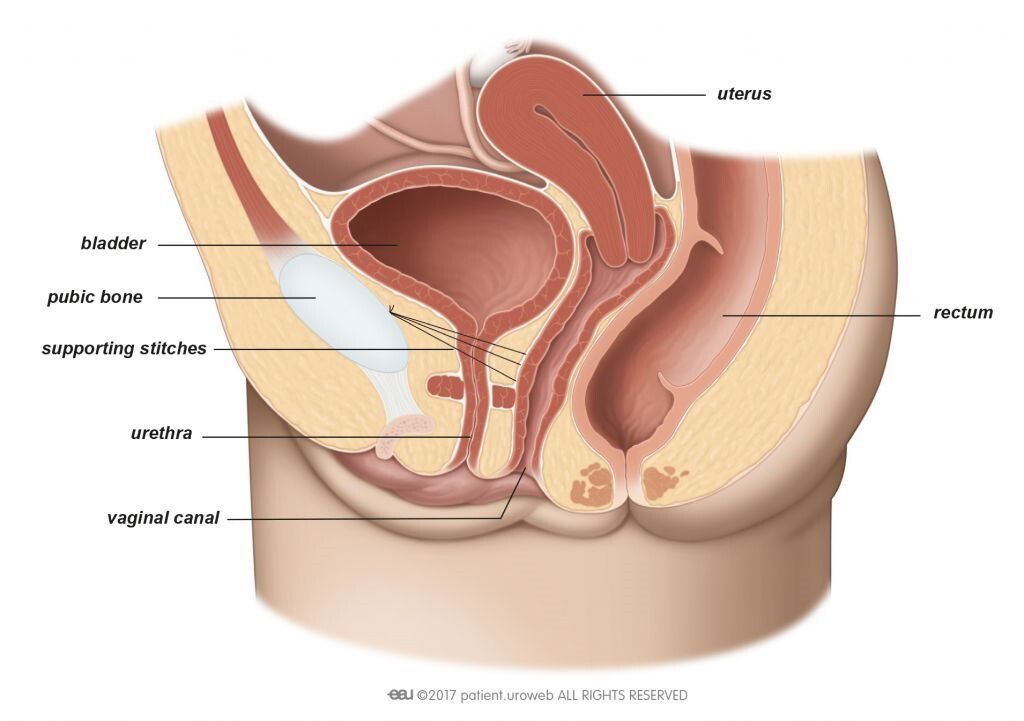
Fig. 1: In Burch colposuspension supporting stitches lift the bladder neck.
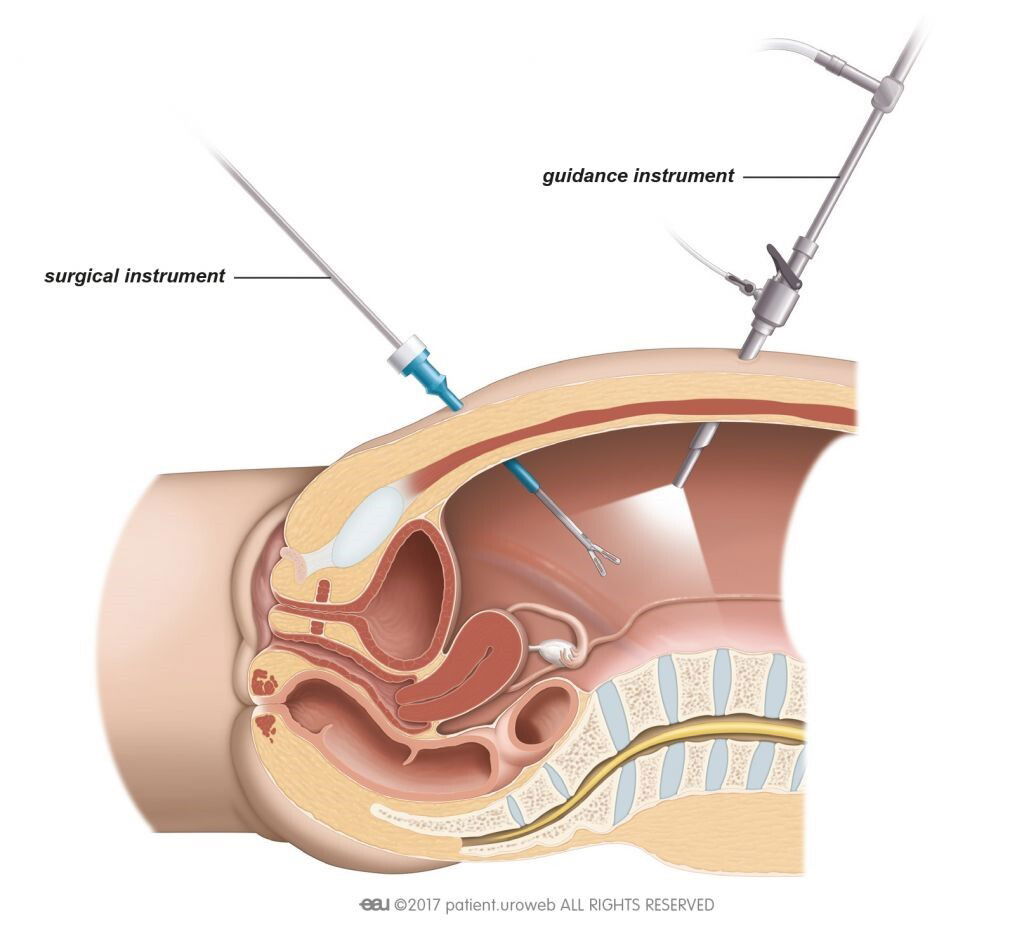
Fig. 2: For laparoscopic surgery the surgeon inserts the surgical instruments through small
incisions in the abdomen.
How do I prepare for the procedure?
Before the surgery the doctor will ask for a urine sample to make sure you do not have a
urinary tract infection. If you have an infection, your doctor will prescribe antibiotics before,
during, and after the operation.
Your doctor will advise you in detail about how to prepare for the procedure. You must not
eat, drink, or smoke for 6 hours before surgery to prepare for the anaesthesia. If you are
taking any prescribed medication, discuss it with your doctor. You may need to stop taking
it several days before surgery. Your doctor will advise you on when to start using it again.
How long will it take me to get back to my daily activities?
The doctor will generally remove the catheter immediately after the surgery and monitor
your recovery. Usually you can leave the hospital a few days after the procedure. If you have problems urinating or there is much residual urine in the bladder, you may have to stay
longer. The recommended length of hospital stay varies in different countries.
Complete recovery from Burch colposuspension may take up to 6 weeks. During this time
you could experience occasional pain in the pelvic area, or pain or a burning sensation
when you urinate. Discuss with your doctor if you can get medication to deal with these
symptoms.
Recommendations for 4-6 weeks after the surgery:
⦁ Drink 1-2 litres every day, especially water
⦁ Do not lift anything heavier than 5 kilograms
⦁ Do not do any heavy exercise
⦁ Take showers instead of baths
⦁ Avoid thermal baths, or going to the sauna
⦁ Adapt your diet to prevent constipation
⦁ Avoid vaginal penetration
You need to go to your doctor or go back to the hospital right away if you:
⦁ Develop a fever
⦁ Are unable to urinate on your own
⦁ Have heavy blood loss or pain
⦁ Notice the wound starts to bleed or leak transparent fluid, or it hurts
Advantages
⦁ High chance of curing SUI by repositioning the bladder neck
⦁ Long-lasting effect
Disadvantages
⦁ Risk of injury to the bladder or the urethra during surgery
⦁ Very low risk of injury to the bowel or blood vessels in the pelvic area
⦁ Risk of temporary urinary retention
⦁ Risk of having pain during sex
Copyright © Clinical Reference Systems 2004
Women's Health Advisor
Copyright © 2004 Elsevier Inc. All rights reserved. www.mdconsult.com